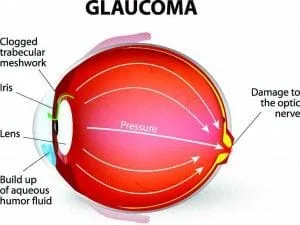
True, Glaucoma does involve the resultant manifestations of too high a pressure within an eye, but this is an over simplification however, as other vascular diseases can increase Glaucomas likelihood and certainly deteriorating health can exasperate this disease even if Intra Ocular pressure seems to be at a pre determined Targeted level therefore this family of diseases the Glaucomas are multi factorial; for the most part of an Inherited Template with 2 identified Genes in the Trabecular meshwork to date. No one is ever cured of Glaucoma but rather managed. Literature would have you know it is the second leading cause of blindness in the US having only the occasional report of blurred vision and the occasional coloured ring around lights even in the Open Angle form. Contrasted to Macular Degeneration that involves the Retinal elements devoted to fine discriminate vision and relating to the central 20 degrees of vision: Glaucoma involves for the largest part of its disease course the retinal tissue that provides the non- discriminate sight. We know that with the disease the first changes occur in the mid-periphery of vision but at the same time a sizable amount of vision loss has occurred before a person realizes they are forming tunnel vision.
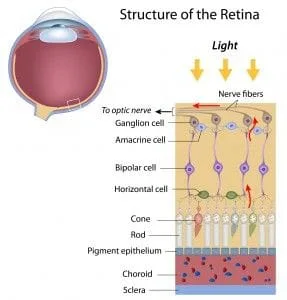
As an aside Data bases are not restricted in Canada in the same way they are in the U.S. by the F.D.A. so OCT’s here have expanded data bases. Macular Ganglion Cell Thinning as a entity gives us the ability to predict glaucoma 3 to 4 years sooner than the HRT. At least this is my experience to date. The Oct seems to indicate Glaucoma 11 to 13 years sooner than other means. A further addition is there is now the Designations PG and PPG. Parametric Glaucoma where a field change occurs and Pre – Parametric where O.N.F.L., optic nerve fiber layer thinning and a loss of Ganglion cells under the macula proceeds any Field or (Parametric Change).
Back to the biomicroscope and digital image method though still useful at this point in order for the next clinician to reach the same conclusion they would run a H.R.T. and expect a similar resultant course. The Humphrey Field Analyzer run annually in this case tests viewing points out to 24 or 30 degrees of the central retina. A cautionary note however is if a defect shows up here it has been determined that 35 to 40% of the fibers have already been damaged if we are talking about pressure only Glaucoma once we factor out fiber loss do to age and omit cardiovascular involvement also.
So if Glaucoma has been determined and a target pressure of low teens has been achieved on going you must still test for progressive loss of nerve fibers. Undetected pressure spikes and blood flow dynamics can alter the disease course. The normal range for IOP is between 11 and 21 mm hg 15.5 being an average.
What does confound many a patient is that they can be told that they have an IOP (intra ocular pressure)) below 20 and at the same time has Glaucoma. This would be considered to be Normal Tension Glaucoma, yes included in the Open Angle Glaucoma family but with a differing etiology. Apparently 61% of Primary Open Angle Glaucoma patients present with a mean pressure below 21 mm Hg. (Optometry Rounds volume 1,issue 4, 2013.)
The held belief is that something is affecting the perfusion pressure to the Optic nerve such that it will be damaged such that a demonstrated field loss will show in the results of parametric, (Field Testing) eventually. The clue- in, to the clinician is changes in Optic nerve head appearance in the early going, possible pressure spikes in serial tonometry: a contact lens called the Trigger fish is coming for this use, isolated disc hemorrhages (‘Drance Hemorrhages’ Lasting up to 3 months) and most importantly confirmable sequenced interval changes on successive HRT tests and now of course the High Def O.C.T.

This will falter with prolonged raised I.O.P. insult and fibers will die. The Cornea with a higher measured Hysteresis value serves a better damper to this strain and because the drug can raise the Hysteresis value it in turn must assist the laminar cribosa matrix slowing what is termed atopsis or fiber melt structural compromise .In these 2 new directives with the Ocular Response analyzer you seem to be dealing more with the Mechanical Theory of Glaucoma and with the Sweapt Source O.C.T. and blood flow tracking at the nerve head the Vascular Theory of Glaucoma.Personally I think they play off each other and are therefore a combined entity.
NOW THE STATS. With regards to Glaucoma just like Diabetes a large portion of the population do not know they have it and just like Diabetes damage can occur before a concrete diagnosis is placed. With Glaucoma it is referred as the “Thief of Sight” as it is never going to give you a clue unlike Diabetes until you are really engaged. Really Shocking Facts: at 65 years of age you are 7 times more likely to have Glaucoma than under that age. Certain ethnic groups approach a near 20% incidence at or around age 75, Hispanic, African American (The Glaucoma research Institute and the Latino eye study). Incidence 1 to 2 % over 40 and about 10% at 70 years of age (UK data). Luckly only 15% go blind. To high by my view. According to a British Study 10% become eventually non responsive to drug therapy and require surgery. Hopefully the ROCK family of drugs and better understanding of blood flow dynamics will reduce the need for surgery as it is not free of complications such as Kissing Choroidals.
Again remember IOP is not the only operative here. Hopefully better monitoring and control measures will reduce this ie: a vaccine as an adjunct treatment. If you have a family member with Glaucoma your risk rose 10 times to 10% if its your sibling who has glaucoma and 4 times to 4% if your mom or dad has or had it. With a Provincial Government in the Province of B.C. that is Clevearly hiding the Rationing of Preventative Diagnostic Eyecare Services by alluding serious Eye Disease only effects those over 60 so they suggest that this segments eyecare is best relgeted to spectacle shops with trumped up auto refractors think again folks. Yes it may be fact that Glaucoma measured with current measures has a realization of 1 % in persons younger than 45 years old. Don’t back away from the fact that a genetic tests once devised could redefine this variable and also take note that from 45 to 60 years of age the incidence jumps by 31% to that under age 45.Questioning now the plausibility that 80% of the people with glaucoma are over 60 years of age and there is the rapid jump after 40? If you chose to buy the Governments argument you will completely ignore the fact that Diabetes is on the rise in Canada attributable to Dietary Choice and a rapidly developing sedentary lifestyle. Know that if you are Myopic to any degree
Irrespective of age your risk for Glaucoma went up. They use to say that Diabetes seemed to give you a 1.8 times greater realization for Glaucoma but Now according to John’s Hopkins and the work done by the Centers for Excellence this statement is INCORRECT. Diabetes is not a risk factor; in fact it may be Neuroprotective by the release of Anti Vegs. Non the less Diabetes is a rapidly expanding biggy of the 4 vision loses CNIB (Canadian National Institute for the Blind) looks at.
When you draw over the entire age Paradim 20 to 70 years of age Diabetic Retinopathy leads as the source of potential vision loss. But it is the leading cause of Vision Loss under 50. According to the C.N.I.B.Of visitations to the CNIB Glaucoma ranks 7.6% and is ascribed a conservative incidence of < 2 %.Half the people that have Glaucoma do not know it.